
GlaucoNova Labs
Smart Eyewear Revolutionizing Glaucoma Management

Revolutionary Eye Care
Ultrasound-Infused eyeglasses for monitoring eye pressure in glaucoma patients continuously at low costs.
The Problem
Problem Framing:
Glaucoma affects 80 million individuals worldwide with a global economic burden of $411 billion. The foremost biomarker is elevated intraocular pressure (IOP), the buildup of aqueous humor damaging optic nerves. Causes underlying this phenomenon are unknown, there exists no cure, and it typically lacks warning symptoms, leading to gradual and "silent" vision loss.

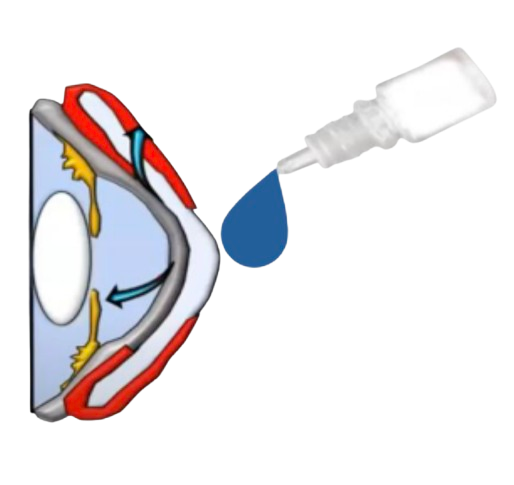
Current Treatments:
Eyedrops are a pervasive treatment to reduce IOP, but their effectiveness is limited by the inability to predict when patients will experience IOP spikes, which can spike 110% beyond normal levels in a matter of seconds at any time of day without one's awareness. This is why 20% of patients become completely blind in at least one eye in 15 years of follow-up.
The Need for Frequent Monitoring:
Despite the need for frequent monitoring, current tonometers are invasive (direct contact with the cornea), non-portable (only found in clinics), and expensive (priced above $1240). They provide a limited snapshot of IOP fluctuations and lead to prescribing ineffective and non-personalized treatment.
Who Are We?
Our Team

Soham Chakraborty
Co-Founder/CEO
Berkeley Bioengineering & Haas School of Business. Product Design, Growth Strategy & Clinical Testing.

Neil Goradia
Co-Founder/CTO
Berkeley Electrical Engineering & Computer Science. Hardware prototyping, PCB Design, IoT & CAD modelling.

Dr. John Flanagan
Senior R&D Advisor
Ex-Dean of Berkeley's College of Optometry. Human testing, IRB, Lab Space & Growth.

George Tanaka
M.D. Strategic Advisor
Glaucoma Specialist & Refractive Cataract Surgeon. Clinical Validation, Sourcing Patient Testimonials & Growth.

Dan Kim
Legal Advisor
Partner Orrick, Herrington & Sutcliffe LLP. IP Acquisition & Entity Incorporation.
Our Technology
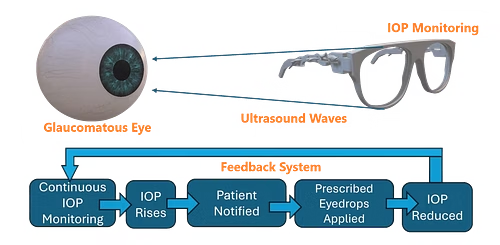
Our innovation, GlaucoSolve Glasses is a non-invasive, wearable, cost-effective, and remote monitoring solution that uses ultrasound transducers, receivers, and Arduino modules to monitor IOP. By applying acoustic force to the cornea and analyzing the reflected signal, we can compute various ultrasound parameters and correlate them to get the patient's eye pressure. Realtime data will be sent to a mobile app allowing physicians to monitor long-term glaucoma progression remotely and alerting patients on when they should apply eye drops, mitigating optic nerve damage. Moreover, we plan to develop a model with collected data, offering AI insights into glaucoma diagnosis. By learning nuanced IOP patterns in patients with all stages of glaucoma, it allows our model to help ophthalmologists spot signs of glaucoma and predict patients' future IOP trajectory to evaluate the effectiveness of treatments just days after prescription.
Our Prototypes

3D Prototype Model
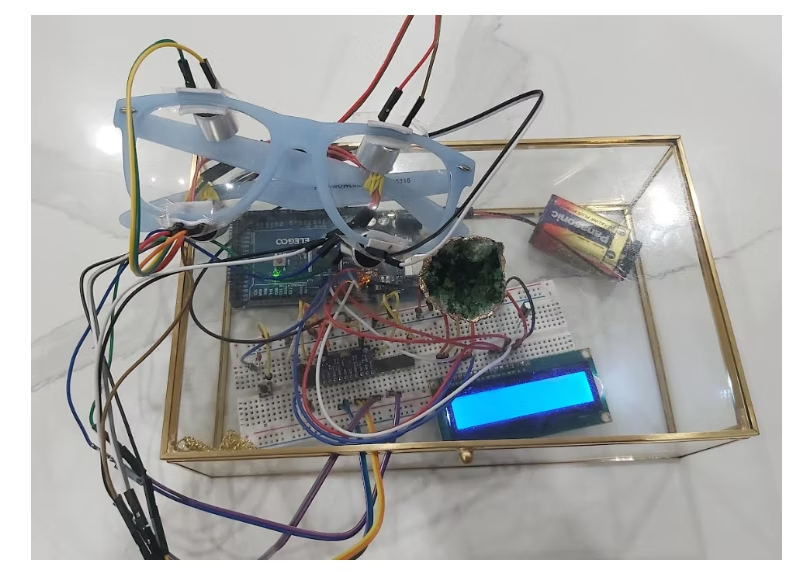
Physical Prototype

V2 Prototype
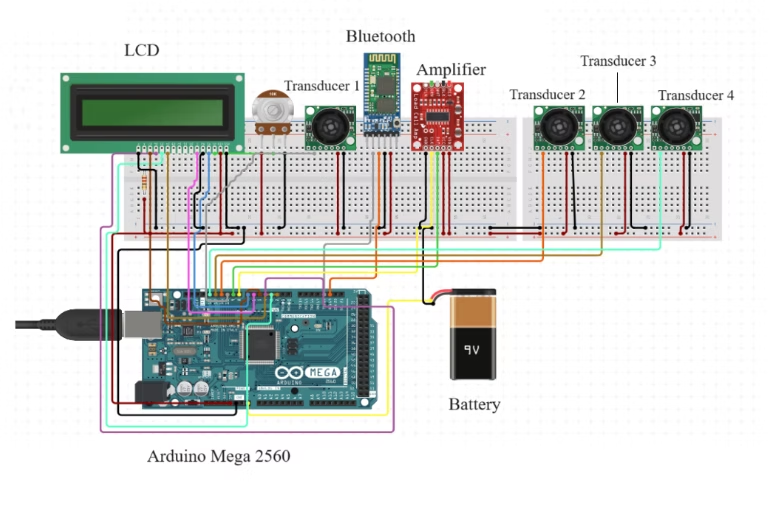
Technology Schematic

Mobile App Interface
V2 Demo
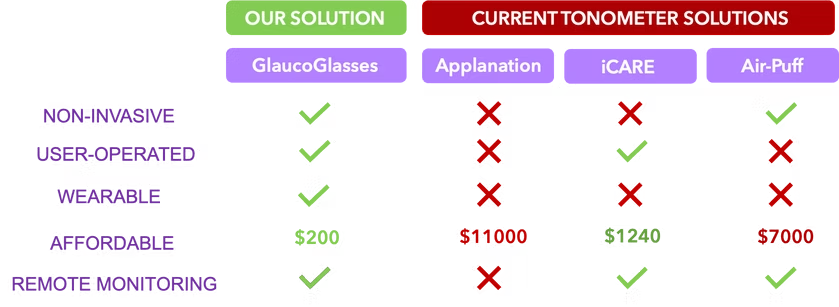
Our Unique Value
So what separates GlaucoSolve from the rest of the IOP monitors? We hold the first wearable technology design capable of continuous IOP monitoring, with a significantly cheaper price point and remote physician monitoring feature. As you can see in the comparison table below, our product outshines each alternative IOP monitor in multiple key factors and is over five times cheaper than the current cheapest option.
The Science Behind GlaucoGlasses
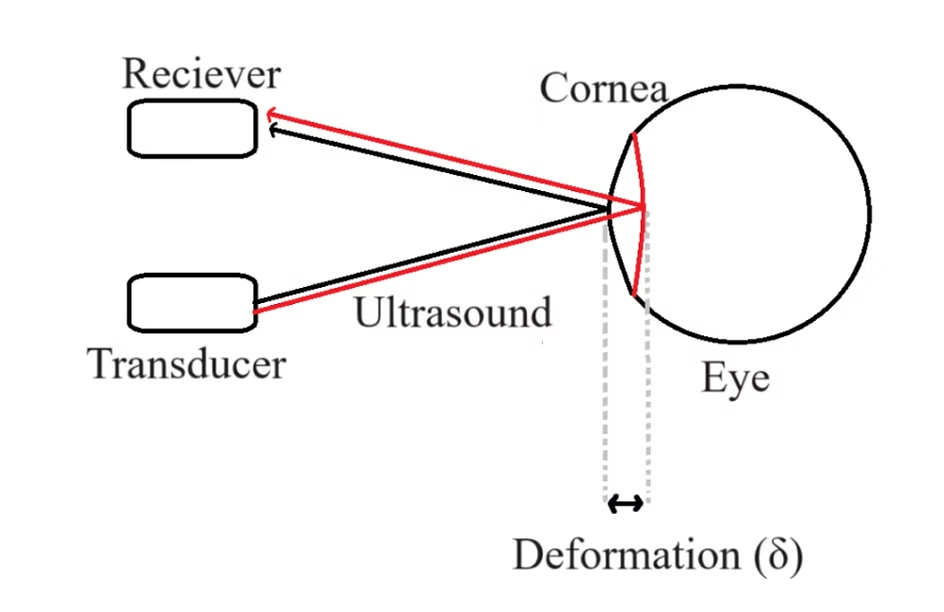
Widely used in elasticity imaging, acoustic radiation force from ultrasound waves induces physical deformation in tissues- elucidating data about the elasticity of the tissue. Applying a known magnitude of acoustic force to the cornea of the eye will similarly enable the measurement of corneal deformation, as shown in Figure 1, offering insights into elasticity, which is known to be correlated to IOP (Lee et al., 2021).
Four variables will be experimentally extracted from the reflected ultrasound signal, which will correlate to IOP. These four parameters are corneal deformation, flight time, amplitude, and acoustic impedance.
Corneal Deformation
The proposed technique to enable the calculation of the final corneal deformation (δ), which is the amount the cornea displaces from its initial position as a result of acoustic radiation force, is the fact that it is the absolute difference between the deformation due to acoustic radiation force and deformation due to IOP. For the average human eye, δ = 38999.76ARFPIOPT - 1116.06, where ARFP is the pressure from acoustic radiation force & IOPT is the true IOP in Pascals (Lee et al., 2021). Thus, corneal deformation should be inversely proportional to IOP, such that higher IOP is correlated with lower corneal deformation, and vice-versa.
Time of Flight
The reflected ultrasound beam from the cornea has two paths: one under normal conditions (black beam in Figure 1) and another during corneal deformation (red beam in Figure 1). Due to the longer distance traveled by the red ultrasound beam, it is expected that the time of flight will be higher during corneal deformation- inversely correlating to IOP (Zhang et al., 2017).
Amplitude
When ultrasonic waves traverse through the air, energy losses, known as attenuation, occur due to scattering, absorption, and density differences at material interfaces. Greater corneal deformation results in longer wave travel, increased acoustic force loss to air, and diminished amplitude, which is the maximum magnitude of received signals, which is expected to be proportional to IOP (Zhang et al., 2017).
Acoustic Impedance
Acoustic Impedance is the resistance against ultrasound wave propagation through tissue, which results from the density of tissue and increases with higher IOP. It is calculated using the equation A1A0 = Z1 - Z0Z1 + Z0, where A0 = a known constant amplitude of signal emitted, A0 = amplitude of signal received, Z0 = acoustic impedance of aqueous humor inside the eye ≈ 1.48 MPa, and Z1 = acoustic impedance of the cornea (Zhang et al., 2017).
Experimental Results
Experimental Setup
After engineering an Arduino-based prototype, experimentation was conducted using the apparatus shown in the image on the right. Since models of the human eye are expensive, the prototype was tested on gelatin phantoms made of gelatin powder and water- an accurate model of biological tissues often used for ultrasound imaging studies. Seven gelatin phantoms, each containing 70 mL of water, with varying gelatin concentrations (10%, 15%, 20%, 25%, 30%, 35%, and 40%) were created to simulate different IOP values of the eye and the ultrasound time of flight and amplitude were extracted for each model. They were then statistically correlated using a linear regression model to the true IOP, which was measured using the iCARE IC100 tonometer, pervasively used in clinics. The results were splendid, yielding a 92% accuracy of IOP correlation with a mean absolute error of solely 5 mmHg. The research paper preprint documenting experimental results is ready to be submitted to Frontiers publication, and the design patent is in the second stage of filing.
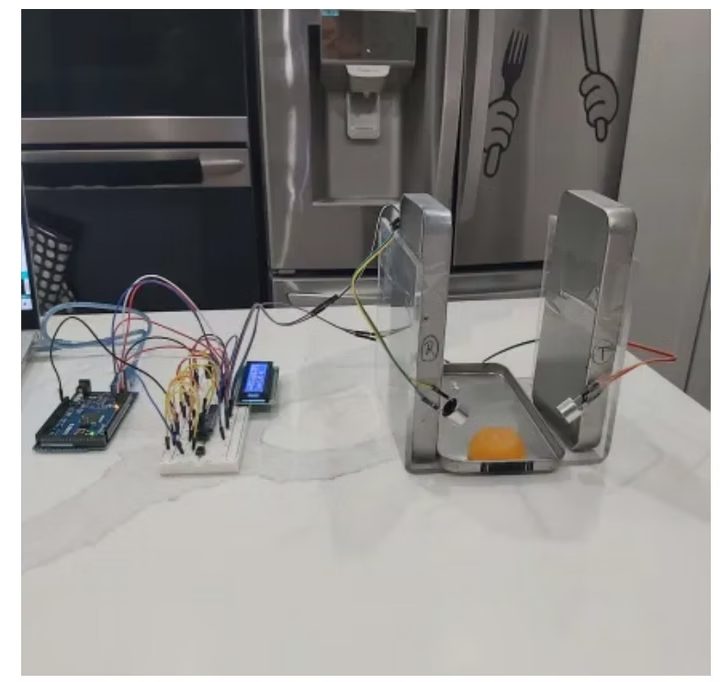
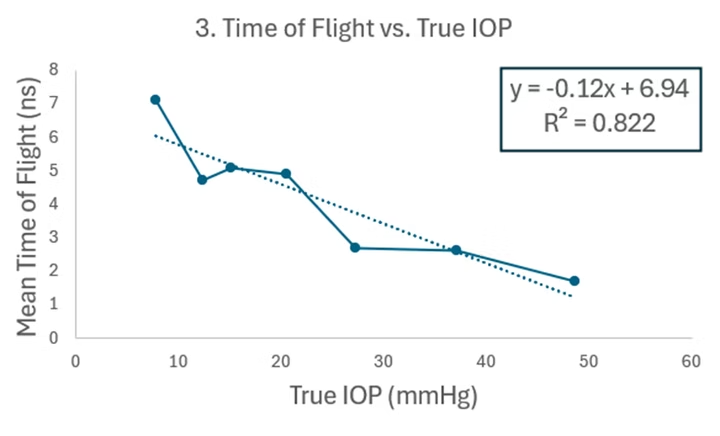
Figure 4: Correlation between time of ultrasound flight in air and true IOP. The time of flight is inversely proportional to IOP, with an 82.2% correlation.
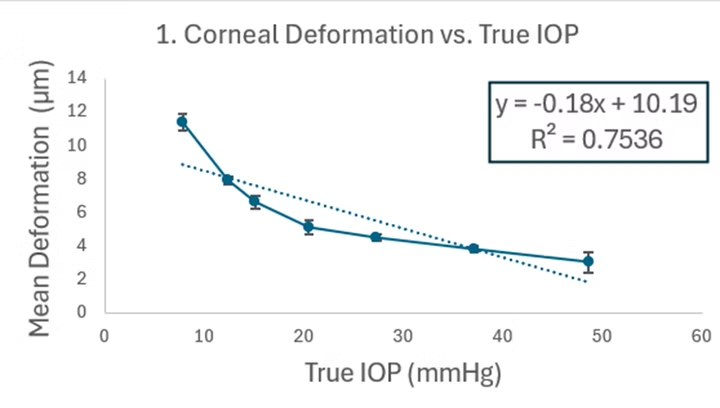
Figure 2: Correlation between corneal displacement and true IOP. Deformation under ultrasound is inversely proportional to IOP with 75.36% correlation.
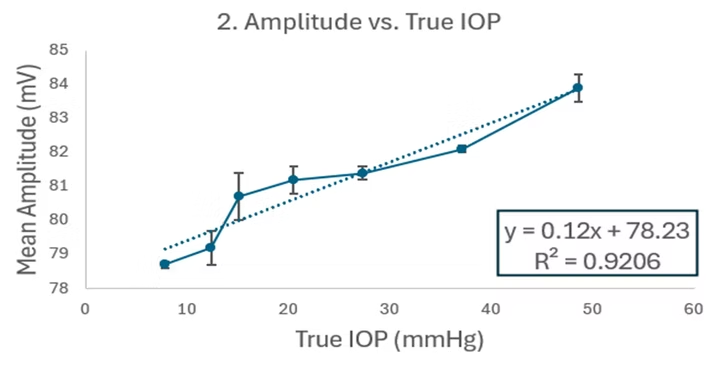
Figure 3: Correlation between ultrasound amplitude and true IOP. Amplitude, the maximum ultrasound signal reflected, is proportional to IOP with 92.06% correlation.
Testimonies
"This product would be very beneficial and useable from the comfort of one's home, reduce the need of going to an eye doctor in person."
Dr. Sewa Ram Singal
General physician at Humber River Hospital and Trillium Health Partners Credit Valley Hospital
"It is a great thinking in this direction as glaucoma is actually a blinding disease."
Dr. Shaffie Baidwal Gupta
Ophthalmologist at Fortis Hospital
Contact Us
Ready to revolutionize your eye health? Get in touch with our team to learn more about GlaucoNova Labs and our innovative technology.
Get In Touch
sohamchakraborty03@gmail.com
Phone
+1 (510) 320-6984
Address
123 Innovation Drive
San Francisco, CA 94105